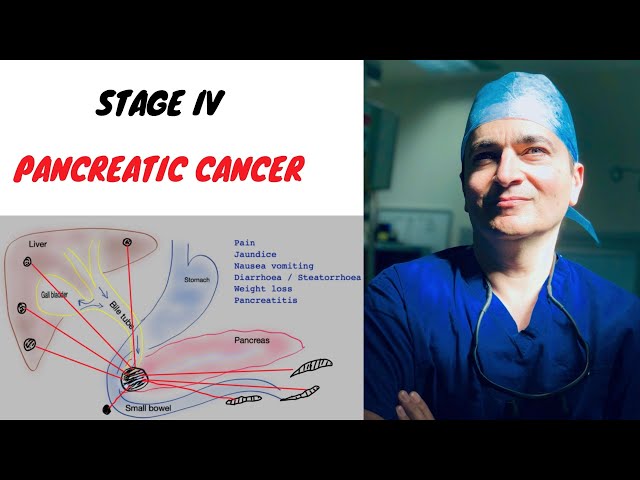
Pancreatic cancer stage 4 treatment is the final stage of treatment for pancreatic cancer, which is a type of cancer that starts in the pancreas. The pancreas is a small organ located behind the stomach that produces enzymes to help digest food and hormones to help control blood sugar levels. Pancreatic cancer stage 4 means that the cancer has spread to other parts of the body, such as the liver, lungs, or bones.
The goal of treatment for pancreatic cancer stage 4 is to relieve symptoms, improve quality of life, and prolong survival. Treatment options may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. The best treatment option for each patient will depend on a number of factors, including the stage of the cancer, the patient’s overall health, and the patient’s preferences.
Pancreatic cancer stage 4 treatment is an important part of managing this disease. By working with a team of doctors and other healthcare professionals, patients can get the best possible care and improve their quality of life.
Pancreatic Cancer Stage 4 Treatment
Pancreatic cancer stage 4 treatment is a critical aspect of managing this disease. It involves various approaches to alleviate symptoms, improve quality of life, and prolong survival. Key aspects of pancreatic cancer stage 4 treatment include:
- Surgery: Removal of the tumor and nearby tissues.
- Chemotherapy: Use of drugs to kill cancer cells.
- Radiation therapy: High-energy rays to shrink tumors.
- Targeted therapy: Drugs that target specific molecules involved in cancer growth.
- Immunotherapy: Enhancing the body’s immune response to fight cancer.
- Palliative care: Managing symptoms and improving quality of life.
These treatments work together to address the advanced stage of the cancer. Surgery can remove the primary tumor, while chemotherapy and radiation therapy target cancer cells that have spread. Targeted therapy and immunotherapy help control cancer growth and boost the immune system. Palliative care provides comfort and support to patients throughout their treatment journey.
Surgery
In pancreatic cancer stage 4 treatment, surgery plays a crucial role in removing the primary tumor and nearby affected tissues. This surgical intervention aims to control the spread of cancer, alleviate symptoms, and improve the patient’s overall quality of life.
- Resection: This primary surgical approach involves removing the tumor along with a margin of healthy tissue surrounding it. The extent of resection depends on the tumor’s location and size.
- Palliative surgery: When complete tumor removal is not feasible, palliative surgery focuses on relieving symptoms and improving quality of life. This may involve bypassing a blocked bile duct or relieving pressure on nerves.
- Minimally invasive surgery: Advanced techniques like laparoscopic and robotic surgery allow for less invasive procedures, resulting in smaller incisions, reduced pain, and faster recovery time.
- Preoperative and postoperative care: Surgery is often combined with other treatments such as chemotherapy or radiation therapy. Preoperative care involves optimizing the patient’s health before surgery, while postoperative care focuses on recovery, pain management, and monitoring for complications.
The decision for surgery in pancreatic cancer stage 4 treatment is carefully considered by a multidisciplinary team of surgeons, oncologists, and other specialists. Factors such as the patient’s overall health, tumor characteristics, and individual preferences are taken into account. Surgery remains an essential component of pancreatic cancer stage 4 treatment, offering potential benefits in symptom control, disease management, and quality of life improvement.
Chemotherapy
Chemotherapy is a vital component of pancreatic cancer stage 4 treatment, playing a crucial role in managing the disease and improving patient outcomes. It involves the administration of powerful drugs to target and kill cancer cells throughout the body.
The significance of chemotherapy in pancreatic cancer stage 4 treatment lies in its ability to control tumor growth, alleviate symptoms, and prolong survival. By targeting rapidly dividing cancer cells, chemotherapy helps shrink tumors, reduce pain, and improve overall quality of life. In some cases, chemotherapy may also be used to prepare patients for surgery or radiation therapy.
The practical application of chemotherapy in pancreatic cancer stage 4 treatment involves a carefully planned regimen tailored to each patient’s individual needs. Treatment plans consider factors such as the stage and location of the cancer, the patient’s overall health, and response to previous therapies. Chemotherapy drugs are typically administered intravenously or orally, and treatment cycles may vary in duration and frequency.
While chemotherapy is an effective treatment for pancreatic cancer stage 4, it can also cause side effects such as nausea, vomiting, hair loss, and fatigue. These side effects are managed through supportive care measures, including anti-nausea medications, hydration, and nutritional support.
In conclusion, chemotherapy remains a cornerstone of pancreatic cancer stage 4 treatment, offering significant benefits in controlling disease progression, alleviating symptoms, and improving patient outcomes. Its integration into personalized treatment plans, along with supportive care measures, ensures optimal management of this complex disease.
Radiation therapy
Radiation therapy is a crucial component of pancreatic cancer stage 4 treatment, utilizing high-energy rays to target and shrink tumors. Its significance lies in its ability to control tumor growth, alleviate symptoms, and improve patient outcomes.
Radiation therapy works by damaging the DNA of cancer cells, leading to their death or preventing their division. In pancreatic cancer stage 4 treatment, radiation therapy can be delivered externally, using a machine that directs beams of radiation to the affected area, or internally, through the placement of radioactive implants near the tumor.
External beam radiation therapy (EBRT) is a common approach, allowing for precise targeting of the tumor while minimizing damage to surrounding healthy tissues. Internal radiation therapy (IRT), also known as brachytherapy, involves placing radioactive seeds or pellets directly into or near the tumor, delivering a high dose of radiation to the specific target area.
Radiation therapy plays a vital role in pancreatic cancer stage 4 treatment, both before and after surgery. It can be used to shrink tumors prior to surgery, making them easier to remove, or to destroy any remaining cancer cells after surgery. Radiation therapy can also be used to relieve pain and other symptoms caused by tumors pressing on nerves or organs.
While radiation therapy is an effective treatment for pancreatic cancer stage 4, it can also cause side effects such as skin irritation, fatigue, and nausea. These side effects are typically temporary and can be managed through supportive care measures.
In conclusion, radiation therapy is an essential component of pancreatic cancer stage 4 treatment, offering significant benefits in controlling tumor growth, alleviating symptoms, and improving patient outcomes. Its integration into personalized treatment plans, along with supportive care measures, ensures optimal management of this complex disease.
Targeted therapy
Targeted therapy plays a significant role in pancreatic cancer stage 4 treatment by precisely targeting specific molecules involved in cancer growth and progression. Unlike traditional chemotherapy, which affects both cancer cells and healthy cells, targeted therapy selectively inhibits the growth and spread of cancer cells while minimizing harm to healthy tissues.
The development of targeted therapy for pancreatic cancer stage 4 treatment is based on a deep understanding of the molecular mechanisms underlying cancer growth. By identifying specific molecules that drive tumor growth, researchers can design drugs that interfere with their function. These drugs can target various molecules, including proteins, enzymes, and receptors, which play crucial roles in cancer cell proliferation, survival, and metastasis.
One example of targeted therapy used in pancreatic cancer stage 4 treatment is erlotinib, which targets the epidermal growth factor receptor (EGFR). EGFR is a protein that promotes cancer cell growth and survival. By blocking EGFR, erlotinib inhibits the growth and spread of cancer cells, thereby improving patient outcomes.
Targeted therapy offers several advantages over traditional chemotherapy. It can be more effective in treating specific types of cancer, has fewer side effects, and allows for more personalized treatment plans. As research continues to uncover the molecular complexities of pancreatic cancer, the development of targeted therapies will continue to play a vital role in improving treatment outcomes for patients with stage 4 disease.
Immunotherapy
Immunotherapy has emerged as a promising treatment approach for pancreatic cancer stage 4, offering a unique way to harness the body’s own immune system to fight cancer. Unlike traditional treatments that directly target cancer cells, immunotherapy aims to stimulate and enhance the immune system’s ability to recognize and destroy cancer cells.
The significance of immunotherapy in pancreatic cancer stage 4 treatment lies in its potential to overcome the challenges posed by this advanced stage of the disease. Pancreatic cancer is often diagnosed at a late stage, when it has spread to other parts of the body, making it difficult to treat with surgery or radiation therapy alone. Immunotherapy offers a systemic approach, targeting cancer cells throughout the body, regardless of their location.
One example of immunotherapy used in pancreatic cancer stage 4 treatment is pembrolizumab, a drug that blocks the PD-1 protein on T cells. PD-1 is a checkpoint protein that normally helps prevent the immune system from attacking healthy cells. By blocking PD-1, pembrolizumab allows T cells to recognize and kill cancer cells more effectively.
The practical significance of understanding the connection between immunotherapy and pancreatic cancer stage 4 treatment lies in the potential to improve patient outcomes. Immunotherapy has shown promising results in clinical trials, extending survival times and improving quality of life for patients with advanced pancreatic cancer. As research continues to uncover the complexities of the immune system and its role in cancer, immunotherapy is expected to play an increasingly important role in the treatment of pancreatic cancer stage 4.
In conclusion, immunotherapy offers a novel and promising approach to pancreatic cancer stage 4 treatment. By harnessing the power of the body’s own immune system, immunotherapy has the potential to overcome the challenges of advanced disease and improve patient outcomes.
Palliative care
In the context of pancreatic cancer stage 4 treatment, palliative care plays a crucial role in managing symptoms and improving quality of life for patients. Palliative care is a specialized medical approach that focuses on providing relief from the physical, emotional, and practical challenges associated with serious illnesses like pancreatic cancer.
The significance of palliative care as a component of pancreatic cancer stage 4 treatment cannot be overstated. As the disease progresses, patients may experience a range of symptoms, including pain, nausea, vomiting, fatigue, and anxiety. These symptoms can significantly impact their quality of life and make it difficult to cope with the challenges of their illness.
Palliative care aims to alleviate these symptoms by providing comprehensive care that addresses the physical, emotional, and spiritual needs of patients and their families. This care may include pain management, nausea control, nutritional support, emotional counseling, and spiritual guidance. By addressing these symptoms and providing holistic support, palliative care helps patients live more comfortably and with greater dignity.
The practical significance of understanding the connection between palliative care and pancreatic cancer stage 4 treatment lies in its ability to improve patient outcomes. Studies have shown that palliative care can reduce pain, improve quality of life, and even prolong survival for patients with advanced cancer. By integrating palliative care into pancreatic cancer stage 4 treatment plans, healthcare providers can ensure that patients receive the best possible care and support throughout their journey.
In conclusion, palliative care is an essential component of pancreatic cancer stage 4 treatment, offering significant benefits in symptom management and quality of life improvement. Its integration into treatment plans ensures that patients receive comprehensive and holistic care, addressing their physical, emotional, and practical needs.
FAQs on Pancreatic Cancer Stage 4 Treatment
This section addresses frequently asked questions about pancreatic cancer stage 4 treatment, providing concise and informative answers to common concerns or misconceptions.
Question 1: What is the goal of treatment for pancreatic cancer stage 4?
The primary goal of treatment for pancreatic cancer stage 4 is to alleviate symptoms, improve quality of life, and prolong survival. Treatment may include a combination of surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, and palliative care.
Question 2: What are the different treatment options available for pancreatic cancer stage 4?
Treatment options for pancreatic cancer stage 4 include surgery to remove the tumor, chemotherapy to kill cancer cells, radiation therapy to shrink tumors, targeted therapy to inhibit specific molecules involved in cancer growth, immunotherapy to enhance the body’s immune response, and palliative care to manage symptoms and improve quality of life.
Question 3: How is the best treatment option determined for each patient?
The best treatment option for each patient with pancreatic cancer stage 4 is determined based on several factors, including the stage and location of the cancer, the patient’s overall health and preferences, and the availability of specific treatments at their treatment center.
Question 4: What are the potential side effects of treatment for pancreatic cancer stage 4?
Treatment for pancreatic cancer stage 4 can cause side effects such as nausea, vomiting, hair loss, fatigue, skin irritation, pain, and decreased appetite. These side effects vary depending on the type of treatment received and the individual patient’s response.
Question 5: How does palliative care fit into the treatment plan for pancreatic cancer stage 4?
Palliative care is an essential component of pancreatic cancer stage 4 treatment, as it focuses on managing symptoms, improving quality of life, and providing support to patients and their families. Palliative care can be provided alongside other treatments, such as chemotherapy or radiation therapy.
Question 6: What is the prognosis for pancreatic cancer stage 4?
The prognosis for pancreatic cancer stage 4 varies depending on individual factors, such as the patient’s age, overall health, and response to treatment. While pancreatic cancer stage 4 is generally considered an advanced stage, advances in treatment have led to improved outcomes and longer survival times for many patients.
Summary: Pancreatic cancer stage 4 treatment involves a multimodal approach to manage symptoms, improve quality of life, and prolong survival. The best treatment option is tailored to each patient’s individual needs and circumstances.
Transition to the next article section: For more in-depth information on pancreatic cancer stage 4 treatment, please refer to the following resources:
Tips for Pancreatic Cancer Stage 4 Treatment
Pancreatic cancer stage 4 treatment can be a challenging journey, but there are proactive steps you can take to improve your experience and maximize the effectiveness of your treatment.
Tip 1: Stay informed about your treatment options.
Educate yourself about the different treatment modalities available, including surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, and palliative care. Knowledge empowers you to make informed decisions about your treatment plan.
Tip 2: Communicate openly with your healthcare team.
Maintain clear and regular communication with your doctors, nurses, and other healthcare providers. Express your concerns, ask questions, and provide feedback. Open dialogue ensures that your needs are met and your treatment plan is tailored to your individual circumstances.
Tip 3: Seek support from loved ones and support groups.
Connect with family, friends, or support groups for emotional support and practical assistance. Sharing your experiences and connecting with others who understand your journey can provide invaluable encouragement and support.
Tip 4: Prioritize your physical and mental well-being.
Engage in activities that promote your physical and mental health, such as exercise, meditation, or spending time in nature. Taking care of your overall well-being can help you cope with the challenges of treatment and improve your quality of life.
Tip 5: Explore complementary therapies.
Consider complementary therapies such as acupuncture, massage, or yoga to supplement your medical treatment. These therapies may help manage symptoms, reduce stress, and enhance your overall sense of well-being. Always discuss complementary therapies with your doctor to ensure they do not interfere with your medical treatment.
Summary: By following these tips, you can proactively participate in your pancreatic cancer stage 4 treatment, improve your experience, and optimize your health and well-being.
Transition to the article’s conclusion: Remember that you are not alone in this journey. Your healthcare team, loved ones, and support groups are there to provide guidance, support, and encouragement every step of the way.
Pancreatic Cancer Stage 4 Treatment
Pancreatic cancer stage 4 treatment encompasses a multifaceted approach to symptom management, quality of life improvement, and survival prolongation. This article has explored the various treatment modalities, ranging from surgery and chemotherapy to targeted therapy and palliative care.
The journey of pancreatic cancer stage 4 treatment is challenging, but advancements in medical research and a comprehensive understanding of the disease offer hope to patients. By staying informed, communicating effectively, seeking support, prioritizing well-being, and exploring complementary therapies, patients can navigate their treatment with greater empowerment and resilience.
As research continues to unravel the complexities of pancreatic cancer and develop innovative treatments, the future outlook for patients is evolving. Continued collaboration between patients, healthcare providers, and researchers is crucial to improve outcomes and enhance the quality of life for those living with this disease.
Youtube Video: